What is Adrenal Fatigue?
Adrenal Fatigue is a collection of signs and symptoms, known as a syndrome that results when the adrenal glands function below the necessary level. Most commonly associated with intense or prolonged stress, it can also arise during or after acute or chronic infections, especially respiratory infections such as influenza, bronchitis or pneumonia. As the name suggests, its paramount symptom is fatigue that is not relieved by sleep but it is not a readily identifiable entity like measles or a growth on the end of your finger. You may look and act relatively normal with adrenal fatigue and may not have any obvious signs of physical illness, yet you live with a general sense of unwellness, tiredness or “gray” feelings. People experiencing Adrenal Fatigue often have to use coffee, colas and other stimulants to get going in the morning and to prop themselves up during the day because they often have mid- morning and mid-afternoon slumps in energy. Conversely, when it comes to bedtime, people with Adrenal Fatigue may have difficulty falling and staying asleep. Although it affects millions of people in the U.S. and around the world, conventional medicine does not yet recognize it as a distinct syndrome.
Adrenal Fatigue can wreak havoc with your life. In the more serious cases, the activity of the adrenal glands is so diminished that you may have difficulty getting out of bed in the morning. With each increment of reduction in adrenal function, every organ and system in your body is more profoundly affected. Changes occur in your carbohydrate, protein and fat metabolism, fluid and electrolyte balance, heart and cardiovascular system, and even sex drive. Many other alterations take place at the biochemical and cellular levels in response to and to compensate for the decrease in adrenal hormones that occurs with adrenal fatigue. Your body does its best to make up for under-functioning adrenal glands, but it does so at a price.
What causes adrenal fatigue?
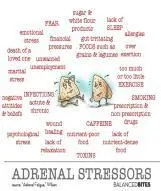
Adrenal Fatigue is produced when your adrenal glands cannot adequately meet the demands of stress.* The adrenal glands mobilize your body’s responses to every kind of stress (whether it’s physical, emotional, inflammatory, psychological, immunological, dietary or environmental) through hormones that regulate energy production and storage, immune function, heart rate, muscle tone, and other processes that enable you to cope with the stress. Whether you have an emotional crisis such as the death of a loved one, a physical crisis such as major surgery, allergies, food sensitivities, hidden or obvious infection or any type of severe repeated or constant stress in your life, your adrenals have to respond to the stress and maintain homeostasis. If their response is inadequate, you are likely to experience some degree of Adrenal Fatigue.
During Adrenal Fatigue your adrenal glands function, but not well enough to maintain optimal homeostasis, because their output of regulatory hormones has been diminished – usually by over-stimulation. Over-stimulation of your adrenals can be caused either by a very intense single stress, or by chronic or repeated stresses that have a cumulative effect.
Who is susceptible to adrenal fatigue?

Anyone can experience Adrenal Fatigue at some time in his or her life. An illness, a life crisis, or a continuing difficult situation can drain the adrenal resources of even the healthiest person. However, there are factors that can make you more susceptible to Adrenal Fatigue. These include certain lifestyles (poor diet, substance abuse, too little sleep and rest, or too many pressures), chronic illness, hidden infections such as viruses, bacterial, fungus or yeast, parasites or repeated infections such as influenza, bronchitis or pneumonia, prolonged situations that you feel trapped or helpless in (bad relationships, stressful jobs, poverty, imprisonment), food allergies or food sensitivities. Maternal adrenal fatigue can occur during gestation.
How can I tell if my adrenals are fatigued?
You may be experiencing adrenal fatigue if you regularly notice one or more of the following:
- You feel tired for no reason and/or burn out.
- You have trouble getting up in the morning, even when you go to bed at a reasonable hour.
- You are feeling rundown or overwhelmed.
- You need caffeine or other stimulants to get going and keep up with the pace of life.
- You have difficulty bouncing back from stress, illness and you’re frequently sick.
- You develop multiple food allergies or food sensitivities.
- You have digestive problems.
- You feel more tired after exercise than energized.
- You crave salty and sweet snacks.
- You get dizziness or light headed while rising.
- You have low blood pressure.
- You have food cravings and weight changes (especially in the abdomen.
- You feel mentally foggy, fuzzy thinking, inability to stay focused.
- You feel more awake, alert and energetic after 6PM than you do all day.
- You have an increased inability to deal with day to day stress, “short fused”, feeling overwhelmed much of the time or you experience anxiety attacks.
- You have loss of sex drive, hormonal issues, severe PMS, hot flashes, perimenopausal symptoms
Can people experiencing adrenal fatigue feel their best again?

Yes, with proper care most people experiencing adrenal fatigue can expect to feel good again. Our Functional Medicine and Diagnostic Nutrition approach to identifying the cause of Adrenal Fatigue, then a step by step approach program in restoring health and vitality has helped thousands of people regain their life back again.
Our Approach to Adrenal Fatigue
Diet – remove dietary stressors, food sensititivies, and replace with foods for individual’s metabolism and needs
Rest – strategic sleeping methods for optimizing energy rejuvenation and bodily repair
Exercise – specialized exercise routines for maximizing vitality and rebuilding adrenal strength
Supplementation – lab guided supplementation to rebuild overall health with specific emphasis on adrenal repair
Stress Reduction – removal of both external and internal stressors and stress reduction techniques are recommended
The Adrenal Glands and Adrenal Fatigue
What are the Adrenal Glands?
The adrenals are two small glands, each weighing 3 to 5 grams, that are located above the kidneys. The adrenals have one of the highest rates of blood flow per gram of tissue, and the highest content of vitamin C per gram of any tissue in the body. The two, walnut-size adrenal glands are the command post of the endocrine system and the glands are located in the small of the back just above the kidneys and underneath the last (twelfth) rib. These small but powerful glands are strategically located in the body near the aorta and vena cava to quickly receive information from the anterior pituitary via the release of Adrenocorticotropic Hormone (ACTH). Despite the small size of the adrenal glands, they are involved in regulating virtually every aspect of body function.
Each adrenal gland is composed of two separate functional entities. The outer zone, or cortex, accounts for 80-90% of the gland and secretes adrenal steroids (cortisol, DHEA-S and aldosterone). The inner zone, or medulla, comprises 10-20% of the gland and secretes the catecholamines (adrenaline and nor-adrenaline). Cortisol, DHEA and adrenaline are the three main adrenal stress hormones. The health and function of these glands have an indirect effect on the production of the hormones such estrogen, testosterone, progesterone, DHEA, cortisone, and pregnenolone. Adrenal hormones also influence insulin function and blood sugar regulation.
The adrenals are also in close proximity to critical organs that the adrenal hormones act upon including the liver, pancreas, kidneys, and others.
Functional Adrenal Stress Testing
Functional Adrenal Stress Testing, by saliva and urine lab assessment, is used to evaluate the adrenal glands and hormone balance. In the event of adrenal exhaustion and imbalances in the reported hormones, underlying causes must be determined, while also supporting the endocrine system with therapies and lifestyle modifications. A vast amount of helpful information can be gathered through Adrenal Gland Testing.
Do you need your Adrenals tested? Adrenal testing is often ordered for individuals who experience the following:
- Chronic stress and stress-related health problems
- Fatigue or lack of energy
- Muscle and joint pain or weakness
- Chronic inflammation
- Blood sugar dysregulation, hypoglycemia
- Osteopenia or osteoporosis
- Insomnia, sleep disturbances or difficulty waking
- Poor memory or difficulty retaining information
- Irritability or mood swings
- Digestive disorders
- Hormonal imbalances
- Changes in skin integrity, easy bruising or excessive stretch marks
- Frequent or chronic infections
- Hypertension
- Increased waist-to-hip ratio or abdominal obesity
- Anxiety or depression
Physiological Effects of the Primary Hormones of the Adrenal Cortex
The adrenal hormones cortisol and DHEA have genetic influence on the body, they penetrate cells and enter the nucleus, where DNA is unlocked and transcribed. Cortisol is the main hormone that directs immune function and its levels are tremendously valuable in assessing overall health. Cortisol and DHEA are also involved in carbohydrate, protein and fat metabolism; eicosanoid modulation; detoxification capacity; endocrine function; and the health of muscle, bone and neural tissues, etc.
Effects of Divergence from Normal Levels of Cortisol and DHEA
Maintaining physiological balance is an important aspect of vibrant health, and nowhere is this more evident when it comes to cortisol. The production of too much cortisol can literally burn up the body, and insufficient cortisol production causes the body’s internal machinery to malfunction, especially at the cellular level.
The adrenal glands produce both cortisol and DHEA in the adrenal cortex under the stimulation of adrenocorticotropic hormone (ACTH), which is released by the pituitary gland. ACTH acts like a whip on the adrenals. It is in many ways similar to a jockey whipping a horse to make it run faster. If the jockey ignores the clues that his horse is fatigued and keeps whipping it, the horse will keep running until it collapses in total exhaustion or death. In the case of the human body, if we allow stress levels to become chronic and out of control, we can sooner or later expect the same result.
Optimal adrenal function exists when the ratio of cortisol to DHEA is in proper balance. This is why measuring this ratio is the best way to both evaluate adrenal function and determine the effects stress is having on overall health. When cortisol levels are elevated and DHEA is low we are considered to be in a Chronic Stress Response. When this happens we are losing (or have already lost) our ability to modulate bodily functions and are on the road to further hormone, immune, and metabolic breakdown. For example, if cortisol levels are too high at night, rather than getting the rest and recovery necessary to maintain optimal physical repair and psychic regeneration, the body will be in a catabolic state (high nighttime cortisol levels inhibit the release of growth hormone necessary to repair and rebuild body tissues). This high cortisol will also have a negative effect on brain function, memory, learning and mood. This is especially true if this condition is ongoing (chronic in nature).
We all have noticed individuals who have excess fat around their hips, thighs or waist and yet they do not seem to be particularly overweight. In fact, these people may be slender except for those “problem” areas. More than making them uncomfortable wearing a bathing suit in public, this unsightly accumulation of fat is a telltale sign of adrenal dysfunction and hormone imbalance, specifically an elevated ratio of cortisol to DHEA.
An elevated cortisol to DHEA ratio will also interfere with the surface integrity of the body’s mucosal linings that act as its first-line immune defense located from the eyes, throat, stomach, intestines to the rectum. This mucosal barrier is primarily under the direction of the adrenal glands, specifically cortisol and DHEA. Cortisol and DHEA systemically modulate the production and turnover of specialized immune cells called immunocytes (also known as plasmacytes) that produce the secretory antibodies that protect us. The primary antibody of defense is secretory IgA (sIgA). When cortisol is elevated and DHEA is low, suppression of these mucosal immune cells occurs, compromising our first-line immune defense, resulting in low sIgA output.
The longer a person is in a state of chronic stress (high ratio of cortisol to DHEA), the more compromised his or her first line of immune defense will be and the greater the risk for opportunistic infections and allergic reactions to foods. This could ultimately lead to cancer, cardiovascular disease as well as autoimmune disease, a variety of degenerative diseases and accelerated aging. In a Chronic Stress Response all body functions have become compromised due to prolonged hormone, immune and metabolic breakdown that can lead like falling dominoes to a cascade of chronic degenerative diseases from which the weakened body has a reduced chance to recover.
Adrenal Gland Testing Can Uncover Three Stages of Adrenal Exhaustion
Stage One: is distinguished by an increase in output of ACTH by the anterior pituitary gland, increased adrenocortical stimulation, increased cortisol output and an increased probability of pregnenolone steal and decreased DHEA. When in a Chronic Stress Response, pregnenolone, the common precursor to cortisol, DHEA and other hormones is preferentially diverted to cortisol production at the expense of the rest of the steroidal hormones. Generally in Stage I cortisol increases and DHEA and its metabolites decrease or an imbalance occurs especially between testosterone and estrogen. Most of these individuals in Stage 1 have good energy and symptoms are rarely present
Stage Two: Adrenal Exhaustion is marked by the transition from increased to decreased cortisol output. This stage is characterized by continuing high levels of ACTH and thus: adrenocortical stimulation, normal total cortisol output, low or borderline low morning, noon or afternoon cortisol levels, normal nighttime cortisol level, and an increased probability of pregnenolone steal and a further decrease in DHEA. This is a transitional phase in which although ACTH stimulation remains high or even increases, the adrenal output of cortisol declines due to the adrenal fatigue associated with continued hyper stimulation. People in Stage II are often symptomatic, experiencing many of the symptoms noted above. In this stage, people begin to self -medicate with coffee and other stimulants, pain medication and sleep aids.
Stage Three: Adrenal Exhaustion is an advanced stage of adrenal exhaustion characterized by decreased total cortisol output. This stage is characterized by continuing high levels of ACTH and thus adrenocortical stimulation, low total cortisol output, and increased probability of a low nighttime cortisol level and pregnenolone steal and even further decrease in DHEA. The adrenal glands are now exhausted to the point that even though there is ongoing hyperstimulation (high ACTH); they continue to lose their capacity and reserve to produce enough cortisol. The eventual result is a crash of the hypothalamic-pituitary-adrenal axis (HPAA) in which essential neuroendocrine feedback loops are unable to return the system to homeostasis. Symptoms from Stage II are now worsening and most people are seeking some type of medical or alternative help to deal with the poor health that has developed from Adrenal Fatigue.
Why is Adrenal Testing Important?
The Adrenal Glands and Adrenal Fatigue
What are the Adrenal Glands?'
per gram of tissue, and the highest content of vitamin C per gram of any tissue in the body. The two, walnut-size adrenal glands are the command post of the endocrine system and the glands are located in the small of the back just above the kidneys and underneath the last (twelfth) rib. These small but powerful glands are strategically located in the body near the aorta and vena cava to quickly receive information from the anterior pituitary via the release of Adrenocorticotropic Hormone (ACTH). Despite the small size of the adrenal glands, they are involved in regulating virtually every aspect of body function.
Each adrenal gland is composed of two separate functional entities. The outer zone, or cortex, accounts for 80-90% of the gland and secretes adrenal steroids (cortisol, DHEA-S and aldosterone). The inner zone, or medulla, comprises 10-20% of the gland and secretes the catecholamines (adrenaline and nor-adrenaline). Cortisol, DHEA and adrenaline are the three main adrenal stress hormones. The health and function of these glands have an indirect effect on the production of the hormones such estrogen, testosterone, progesterone, DHEA, cortisone, and pregnenolone. Adrenal hormones also influence insulin function and blood sugar regulation.
The adrenals are also in close proximity to critical organs that the adrenal hormones act upon including the liver, pancreas, kidneys, and others.
Functional Adrenal Stress Testing
Functional Adrenal Stress Testing, by saliva and urine lab assessment, is used to evaluate the adrenal glands and hormone balance. In the event of adrenal exhaustion and imbalances in the reported hormones, underlying causes must be determined, while also supporting the endocrine system with therapies and lifestyle modifications. A vast amount of helpful information can be gathered through Adrenal Gland Testing.
Do you need your Adrenals tested? Adrenal testing is often ordered for individuals who experience the following:
- Chronic stress and stress-related health problems
- Fatigue or lack of energy
- Muscle and joint pain or weakness
- Chronic inflammation
- Blood sugar dysregulation, hypoglycemia
- Osteopenia or osteoporosis
- Insomnia, sleep disturbances or difficulty waking
- Poor memory or difficulty retaining information
- Irritability or mood swings
- Digestive disorders
- Hormonal imbalances
- Changes in skin integrity, easy bruising or excessive stretch marks
- Frequent or chronic infections
- Hypertension
- Increased waist-to-hip ratio or abdominal obesity
- Anxiety or depression
Physiological Effects of the Primary Hormones of the Adrenal Cortex
The adrenal hormones cortisol and DHEA have genetic influence on the body, they penetrate cells and enter the nucleus, where DNA is unlocked and transcribed. Cortisol is the main hormone that directs immune function and its levels are tremendously valuable in assessing overall health. Cortisol and DHEA are also involved in carbohydrate, protein and fat metabolism; eicosanoid modulation; detoxification capacity; endocrine function; and the health of muscle, bone and neural tissues, etc.
Effects of Divergence from Normal Levels of Cortisol and DHEA
Maintaining physiological balance is an important aspect of vibrant health, and nowhere is this more evident when it comes to cortisol. The production of too much cortisol can literally burn up the body, and insufficient cortisol production causes the body’s internal machinery to malfunction, especially at the cellular level.
The adrenal glands produce both cortisol and DHEA in the adrenal cortex under the stimulation of adrenocorticotropic hormone (ACTH), which is released by the pituitary gland. ACTH acts like a whip on the adrenals. It is in many ways similar to a jockey whipping a horse to make it run faster. If the jockey ignores the clues that his horse is fatigued and keeps whipping it, the horse will keep running until it collapses in total exhaustion or death. In the case of the human body, if we allow stress levels to become chronic and out of control, we can sooner or later expect the same result.
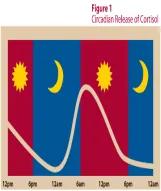
Optimal adrenal function exists when the ratio of cortisol to DHEA is in proper balance. This is why measuring this ratio is the best way to both evaluate adrenal function and determine the effects stress is having on overall health. When cortisol levels are elevated and DHEA is low we are considered to be in a Chronic Stress Response. When this happens we are losing (or have already lost) our ability to modulate bodily functions and are on the road to further hormone, immune, and metabolic breakdown. For example, if cortisol levels are too high at night, rather than getting the rest and recovery necessary to maintain optimal physical repair and psychic regeneration, the body will be in a catabolic state (high nighttime cortisol levels inhibit the release of growth hormone necessary to repair and rebuild body tissues). This high cortisol will also have a negative effect on brain function, memory, learning and mood. This is especially true if this condition is ongoing (chronic in nature).
We all have noticed individuals who have excess fat around their hips, thighs or waist and yet they do not seem to be particularly overweight. In fact, these people may be slender except for those “problem” areas. More than making them uncomfortable wearing a bathing suit in public, this unsightly accumulation of fat is a telltale sign of adrenal dysfunction and hormone imbalance, specifically an elevated ratio of cortisol to DHEA.
An elevated cortisol to DHEA ratio will also interfere with the surface integrity of the body’s mucosal linings that act as its first-line immune defense located from the eyes, throat, stomach, intestines to the rectum. This mucosal barrier is primarily under the direction of the adrenal glands, specifically cortisol and DHEA. Cortisol and DHEA systemically modulate the production and turnover of specialized immune cells called immunocytes (also known as plasmacytes) that produce the secretory antibodies that protect us. The primary antibody of defense is secretory IgA (sIgA). When cortisol is elevated and DHEA is low, suppression of these mucosal immune cells occurs, compromising our first-line immune defense, resulting in low sIgA output.
The longer a person is in a state of chronic stress (high ratio of cortisol to DHEA), the more compromised his or her first line of immune defense will be and the greater the risk for opportunistic infections and allergic reactions to foods. This could ultimately lead to cancer, cardiovascular disease as well as autoimmune disease, a variety of degenerative diseases and accelerated aging. In a Chronic Stress Response all body functions have become compromised due to prolonged hormone, immune and metabolic breakdown that can lead like falling dominoes to a cascade of chronic degenerative diseases from which the weakened body has a reduced chance to recover.
Adrenal Gland Testing Can Uncover Three Stages of Adrenal Exhaustion
Stage One:is distinguished by an increase in output of ACTH by the anterior pituitary gland, increased adrenocortical stimulation, increased cortisol output and an increased probability of pregnenolone steal and decreased DHEA. When in a Chronic Stress Response, pregnenolone, the common precursor to cortisol, DHEA and other hormones is preferentially diverted to cortisol production at the expense of the rest of the steroidal hormones. Generally in Stage I cortisol increases and DHEA and its metabolites decrease or an imbalance occurs especially between testosterone and estrogen. Most of these individuals in Stage 1 have good energy and symptoms are rarely present
Stage Two:Adrenal Exhaustion is marked by the transition from increased to decreased cortisol output. This stage is characterized by continuing high levels of ACTH and thus: adrenocortical stimulation, normal total cortisol output, low or borderline low morning, noon or afternoon cortisol levels, normal nighttime cortisol level, and an increased probability of pregnenolone steal and a further decrease in DHEA. This is a transitional phase in which although ACTH stimulation remains high or even increases, the adrenal output of cortisol declines due to the adrenal fatigue associated with continued hyper stimulation. People in Stage II are often symptomatic, experiencing many of the symptoms noted above. In this stage, people begin to self -medicate with coffee and other stimulants, pain medication and sleep aids.
Stage Three:Adrenal Exhaustion is an advanced stage of adrenal exhaustion characterized by decreased total cortisol output. This stage is characterized by continuing high levels of ACTH and thus adrenocortical stimulation, low total cortisol output, and increased probability of a low nighttime cortisol level and pregnenolone steal and even further decrease in DHEA. The adrenal glands are now exhausted to the point that even though there is ongoing hyperstimulation (high ACTH); they continue to lose their capacity and reserve to produce enough cortisol. The eventual result is a crash of the hypothalamic-pituitary-adrenal axis (HPAA) in which essential neuroendocrine feedback loops are unable to return the system to homeostasis. Symptoms from Stage II are now worsening and most people are seeking some type of medical or alternative help to deal with the poor health that has developed from Adrenal Fatigue.
The chart below illustrates the progressive stages of Adrenal Fatigue.
Common Adrenal Stressors
The Adrenal Rhythm and Its Importance
Energy Production:
The maintenance of a stable blood sugar level depends on food choice, lifestyle, adrenal function and insulin activity. Advanced Adrenal Gland Testing measures not only stress hormones, but insulin can be added to help ferret out the causes of fatigue, sugar cravings and obesity.
Muscle and Joint Function:
Abnormal adrenal rhythms are known to compromise tissue healing. Reduced tissue repair and increased tissue breakdown can lead to muscle and joint wasting with chronic pain.
Bone Health:
The adrenal rhythm determines how well we build bone. If the night and morning cortisol levels are elevated, our bones do not rebuild well, and we are more prone to osteoporosis. Stress is the enemy of the bones. In postmenopausal women, the effect of stress worsens due to female hormone imbalances.
Immune Health:
Various immune cells (white blood cells) cycle in and out of the spleen and bone marrow. The immune system trafficking follows the cortisol cycle. If the cycle is disrupted, especially at night, then the immune system is adversely affected. Short- and long-term stress is known to suppress the immune response in the lungs, throat, urinary tract and intestines. With reduction in the surface antibody (called secretory IgA), the resistance to infection is reduced and allergic reactions are believed to increase. Special “Secretory IgA” testing is often added to evaluate this important bodily component.
Sleep Quality:
The ability to enter REM sleep cycles and experience regenerative sleep is interrupted by high cortisol values at night and in the morning. Chronic lack of REM sleep can reduce a person’s mental vitality, vigor and induce depression.
Skin Regeneration:
Human skin regenerates mostly during the night. With higher night cortisol values, less skin regeneration takes place. Therefore a normal cortisol rhythm is essential for optimal skin health.
Thyroid Function:
The level of cortisol at the cell level controls thyroid hormone production. Often, hypothyroid symptoms such as fatigue and low body temperature are due to an adrenal maladaptation.
Chronic Fatigue Syndrome (CFS):
A common HPA axis defect in CFS is impaired corticotrophin release. As a result, low cortisol and eventual adrenal atrophy may be observed. Depleted adrenals with flat rhythms are often seen on the Adrenal Gland Testing. Simultaneous use of several therapies can help improve the debilitating effects of CFS.
Glycemic Dysregulation:
Chronic hypoglycemia ( low blood sugar) can impair normal adrenal function by repetitive overstimulation of cortisol production. Recurring exposure to high cortisol will impair insulin activity, and invariably lead to insulin resistance and beta-cell exhaustion (diabetes). Adrenal Gland Testing investigates the insulin-cortisol relationship under real-life conditions to allow targeted and meaningful interventions. This testing is useful in the following clinical situations: rapid weight gain and obesity, deranged blood lipids, sugar blues, early diabetes and associated emotional disturbances.
Allergies/Autoimmune Disorders:
More than fifty years ago, Dr. W. Jefferies (author of Safe Uses of Cortisol) discovered that patients with environmentally triggered allergies and autoimmune diseases dramatically benefited when given cortisol for other purposes. More recently, German researchers reported that disruption of the adrenal axis and cytokine relationships lead to predisposition and aggravation of autoimmune diseases. The findings of the Adrenal Gland Testing help identify patients with autoimmune diseases and adrenal problems who can benefit from cortisol supplements.
Depression/ADD:
Several recent publications report a hyperactive HPA axis in depressed patients. Elevated midnight salivary cortisol is now considered one of the best tests in diagnosing endogenous depression. Other anomalies in cortisol rhythm usually accompany the midnight elevation. On the other hand, cortisol elevations and rhythm disruptions throughout the day are typical of attention deficit disorders (ADD).
The chart below illustrates the progressive stages of Adrenal Fatigue.
Contact us at: 609-484-9300 . . . we can help!
Dr. Joseph Gitto
Advanced Chiropractic Techniques
Functional Medicine and Diagnostic Nutrition
